INTRODUCTION
The COVID-19 Pandemic
On March 11, 2020, the World Health Organization (WHO) declared a global pandemic because of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), commonly known as COVID-19.1 The world had to rapidly adapt to the constant change in restrictions and policies to limit the transmission of the virus.1 In Ontario, the provincial government implemented public health measures such as gathering restrictions, physical distancing, work-from-home policies, suspension and delay of many health care services, increase in virtual health care, and mandatory use of face masks in indoor public spaces.2 COVID-19 had widespread health effects across communities. Public Health Ontario epidemiological reports found that marginalized communities in the most materially deprived neighbourhoods and the most ethnically diverse neighbourhoods in Ontario experienced higher rates of COVID-19 infection, more severe outcomes, and higher mortality rates.3,4
Chest/breastfeeding rates during the COVID-19 Pandemic
Chest/breastfeeding has many well-known health benefits. The WHO, Health Canada, and the Canadian Paediatric Society recommend exclusive chest/breastfeeding for the first 6 months with continued chest/breastfeeding for up to 2 years and beyond.5–7 The benefits of chest/breastfeeding for the newborn include protection against gastrointestinal and respiratory infections, protection against sudden infant death syndrome, and enhanced cognitive development.6–10 Chest/breastfeeding protects against breast cancer, ovarian cancer, and type 2 diabetes for the chest/breastfeeding parent.6,8,10 In June 2020, the WHO recommended that chest/breastfeeding be initiated and continued in spite of a suspected or confirmed COVID-19 infection, as the risk of transmission of the virus to the infant was found to be low.11 Newer research has demonstrated that chest/breastfeeding provides newborns with immunity against COVID-19 because of the presence of antibodies found in human milk.12
In spite of the COVID-19 pandemic, chest/breastfeeding intentions during pregnancy remained high around the world.13 Yet, the impacts of the COVID-19 restrictions on chest/breastfeeding rates are mixed. In a United Kingdom sample, chest/breastfeeding rates remained comparable to pre-pandemic rates.14 Similarly, an international cross-sectional study found that COVID-19-imposed changes in perinatal care did not affect chest/breastfeeding rates.15 However, the same study found that virtual support groups were positively associated with continued chest/breastfeeding at 6 months, particularly for parents with their first child.15 They also found that a lack of support negatively affected chest/breastfeeding rates.15 Others found that the COVID-19 pandemic public health restrictions mostly had negative impacts on chest/breastfeeding such as separation of parent and infant, lack of skin to skin contact, and insufficient postpartum support.16 Another study found the most common reason for chest/breastfeeding cessation during the COVID-19 pandemic was the lack of professional face-to-face support.17
There were also some unexpected positive impacts of the pandemic restrictions mainly reported by participants with higher socioeconomic status, which included protecting the chest/breastfeeding parent–infant dyad from unwanted visitors at home, more time to focus on chest/breastfeeding, and greater support from their partner with delayed return to work outside the home.16
The Standard Ontario Midwifery Postpartum Care Visit Schedule
The Ontario midwifery model of postpartum care provides high-quality primary care for the parent– infant dyad from birth to 6 weeks postpartum. The hallmarks of this model are multiple visits, visits in the client’s preferred setting (home, hospital, or clinic), and individualized dyad-centered care.18 Midwives provide clinical care for the parent and newborn, and support mental health well-being, infant growth and development, chest/breastfeeding, and parent-infant bonding. A typical postpartum visit schedule includes three to five visits in home or hospital and one to three clinic visits.18 In 2016–2017, midwives in Ontario provided an average of 6.6 postpartum visits per client with a range from 0–25 visits.18 The College of Midwives of Ontario rescinded the 2015 Postpartum/newborn Visits Standard19 in 2018, to better support midwives to use their clinical judgment and adjust the postpartum visit schedule to respond to the needs of clients.18 The Ontario midwifery postpartum care model has resulted in excellent health outcomes for both parents and infants, including high chest/breastfeeding rates at 6 weeks postpartum,18 high client satisfaction,18 and reduced unscheduled postpartum hospital emergency department use.20
Alternative Ontario Midwifery Postpartum Care Visit Schedule
Beginning in March 2020, the Association of Ontario Midwives (AOM) proposed an alternative midwifery postpartum visit schedule to reduce COVID-19 exposure and community transmission using guidance from the WHO.21 The alternative schedule proposed one in-person visit within 48 hours of birth, at least one additional in-person visit in the first week, and additional virtual visits, including the discharge visit, by phone or videoconference.21 Health precautions were recommended for clinical situations that required an in-person assessment by the midwife.
OBJECTIVE
This study aims to determine whether the alternative midwifery postpartum visit schedule imposed by the COVID-19 pandemic affected the chest/breastfeeding rate of midwifery clients compared to the standard postpartum visit schedule.
METHOD
Setting
Seventh Generation Midwives Toronto (SGMT) is an Indigenous-led midwifery practice group of Indigenous registered midwives, Indigenous midwives working under an exemption of the Midwifery Act, and non-Indigenous registered midwives located in Toronto, Ontario.
Design
Literature Review
A literature review was conducted from August 2022 to 2024 using the following databases: Cochrane Library, PubMed MEDLINE, Ovid MEDLINE, Cumulative Index to Nursing & Allied Health (CINAHL) EBSCO, the Toronto Metropolitan University Libraries, and Google Scholar. The main search terms included: “midwi* AND postpartum AND (visit OR schedule) AND (breastfeed* OR infant feed* OR lact*) AND COVID,” with a preference for relevant articles in Ontario, Canada. The database search limits were English language and peer-reviewed articles. To our knowledge, this study is the first to research the Ontario midwifery postpartum visit schedule and its effect on breastfeeding rates during the COVID-19 pandemic. The literature review found no relevant studies.
Study Design
This is a quantitative retrospective cohort study of midwifery care for clients who gave birth before or during the COVID-19 pandemic and had 6 weeks of postpartum care with SGMT midwives. The primary outcome is chest/breastfeeding status at 6 weeks postpartum, described as exclusive chest/breastfeeding, combined feeding (chest/breastfeeding and formula feeding), or exclusive formula feeding. The secondary outcomes include (1) the mean number of postpartum visits, (2) the type of postpartum visits, (3) feeding status at Day 3 postpartum, (4) feeding status at 2 weeks postpartum, and (5) the percentage of midwifery clients accessing additional chest/breastfeeding support.
Participants
Exclusion Criteria
Midwifery clients with any of the following conditions were excluded from the study: (1) stillbirth, (2) preterm birth less than 37+0 weeks gestation, (3) neonatal intensive care (NICU) admission, (4) severe postpartum hemorrhage (>1000 mL), (5) hypertensive disorders of pregnancy, (6) preexisting or gestational diabetes, (7) maternal hospital readmission in the postpartum period, or (8) twin pregnancies.
Sample Size
Using purposive sampling, 300 anonymized client charts, 150 in each cohort, were included to detect a statistically significant change of 10% in the chest/breastfeeding rate for a type-I error of 5% and a power of 90%.
Data Collection
A total of 300 midwifery clients (N = 300) passed the exclusion criteria, and data from their Ontario perinatal records and postnatal records were collected and anonymized. The pre-pandemic cohort (n1 = 150) gave birth between January 1, 2018 and October 31, 2018. The pandemic cohort (n2 = 150) gave birth between April 1, 2020 and November 30, 2020.
Data Analysis
The baseline characteristics and study outcomes were compared between the two cohorts to identify potential confounding variables. Continuous variables were compared using the independent t-test. Variance in continuous variables was compared using the F-test. Categorical variables were compared using the Chi-square test. Multivariable logistic regression analysis was used to determine whether the type of postpartum schedule was associated with any chest/breastfeeding rate differences while adjusting for potential confounding factors. The results are presented as an adjusted odds ratio (aOR) with a 95% confidence interval (95% CI).
Ethics Approval
The DAN Women & Babies Program Research Committee and the Sunnybrook Research Ethics Board reviewed and approved this study, project identification #5409.
RESULTS
Demographics
The pre-pandemic cohort consisted of 150 midwifery clients who gave birth between January and October 2018, while the pandemic cohort consisted of 150 clients who gave birth between April and November 2020. The demographics of the two cohorts are shown below in Table 1. There were no significant differences in age and ethnicity between the cohorts. The pandemic cohort had 16.0% more primiparous clients and 16.7% more clients without chest/breastfeeding experience than the pre-pandemic cohort. Since the primiparous clients had no chest/breastfeeding experience, the higher percentage of primiparous clients without chest/breastfeeding experience in the pandemic cohort was the main significant difference between the cohorts. The pandemic cohort also had a statistically significant 9.3% increase in home births.
Table 1. Demographic characteristics of the pre-pandemic cohort and the pandemic cohort.
| Characteristic | Pre-pandemic cohort (n1= 150) Frequency (%) | Pandemic cohort (n2= 150) Frequency (%) | p-value (α < 0.05) |
|---|---|---|---|
| Age at delivery, mean (years ± SD) | 32 ± 4.960 | 33 ± 4.444 | 0.067 |
| Age at delivery, range (years) | 19 to 45 | 18 to 47 | 0.091 |
| Ethnicity | 0.441 | ||
| White/European | 70 (46.7%) | 76 (50.7%) | |
| First Nations/Métis/Inuit/Mixed | 22 (14.7%) | 12 (8.0%) | |
| East/Southeast Asian | 17 (11.3%) | 16 (10.7%) | |
| Black/Caribbean | 9 (6.0%) | 8 (5.3%) | |
| Latin/Central/South American | 7 (4.7%) | 12 (8.0%) | |
| South Asian | 6 (4.0%) | 6 (4.0%) | |
| West Asian | 2 (1.3%) | 6 (4.0%) | |
| Multiple Ethnicities | 17 (11.3%) | 14 (9.3%) | |
| Parity* | 0.005 | ||
| Primiparous | 58 (38.7%) | 82 (54.7%) | |
| Multiparous | 92 (61.3%) | 68 (45.3%) | |
| Chest/breastfeeding experience* | 0.004 | ||
| No chest/breastfeeding experience | 59 (39.3%) | 84 (56.0%) | |
| Previous chest/breastfeeding experience | 91 (60.7%) | 66 (44.0%) | |
| Birth location* | 0.016 | ||
| Sunnybrook Health Sciences Centre | 115 (76.7%) | 104 (69.3%) | 0.153 |
| Toronto Birth Centre | 29 (19.3%) | 26 (17.3%) | 0.654 |
| Home* | 6 (4.0%) | 20 (13.3%) | 0.004 |
SD, standard deviation; *, statistically significant difference p < 0.05.
Chest/Breastfeeding Rates
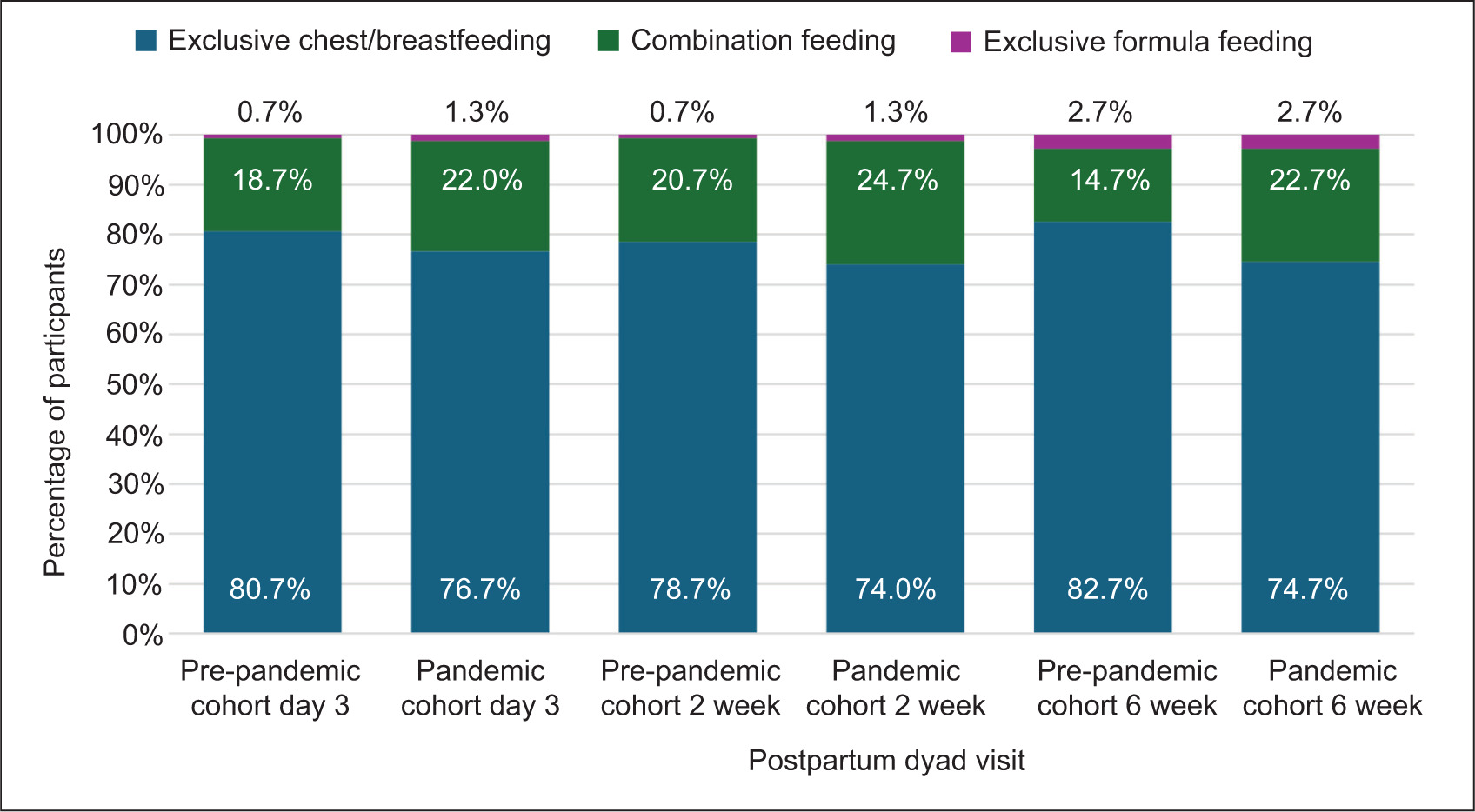
The exclusive chest/breastfeeding rate at 6 weeks postpartum was 82.7% in the pre-pandemic cohort and 74.7% in the pandemic cohort (Figure 1); an 8.0% decline during the pandemic but not statistically significant. The pandemic cohort had an 8.0% increase in combination feeding at 6 weeks postpartum compared to the pre-pandemic cohort. The exclusive formula feeding rate at 6 weeks postpartum was the same for both cohorts at 2.7%. There were no statistically significant differences between cohorts for exclusive chest/breastfeeding, combination feeding, and formula feeding rates at Day 3 and 2 weeks postpartum (Figure 1).
Figure 1. Chest/breastfeeding rates at Day 3, 2 weeks, and 6 weeks postpartum of the pre-pandemic cohort and pandemic cohort.
Midwifery Postpartum Visit Schedule
In the pre-pandemic cohort, midwives provided an average of six postpartum visits with a standard deviation of ± 1 similar to the standard midwifery postpartum visit schedule. The range of the number of postpartum visits provided was four to eight visits (Table 2). During the pandemic, the average number of total postpartum visits provided by the midwives remained the same as before the pandemic, but there was a greater variation in the range of total number of postpartum visits from three to nine visits (Table 2).
Table 2. Total number of postpartum visits before and during the COVID-19 pandemic.
| Measurement | Pre-pandemic cohort (n1= 150) | Pandemic cohort (n2= 150) |
|---|---|---|
| Total number of postpartum visits, mean ± SD | 6 ± 0.872 | 6 ± 1.197 |
| Total number of postpartum visits, range | 4 to 8 | 3 to 9 |
SD, standard deviation; p-value = 1.000.
In the pre-pandemic cohort, over 99% of the postpartum visits were in-person, while virtual visits made up less than 1% of the total (Table 3). Similarly, in the pandemic cohort, 99% of the postpartum visits were in-person while less than 1% were virtual (Table 3).
Table 3. Percentage of in-person and virtual postpartum visits before and during the COVID-19 pandemic.
| Measurement | Pre-pandemic cohort | Pandemic cohort |
|---|---|---|
| Percentage of in-person postpartum visits | 99.89% | 99.4% |
| Percentage of virtual postpartum visits | 0.11% | 0.6% |
p-value = 1.000.
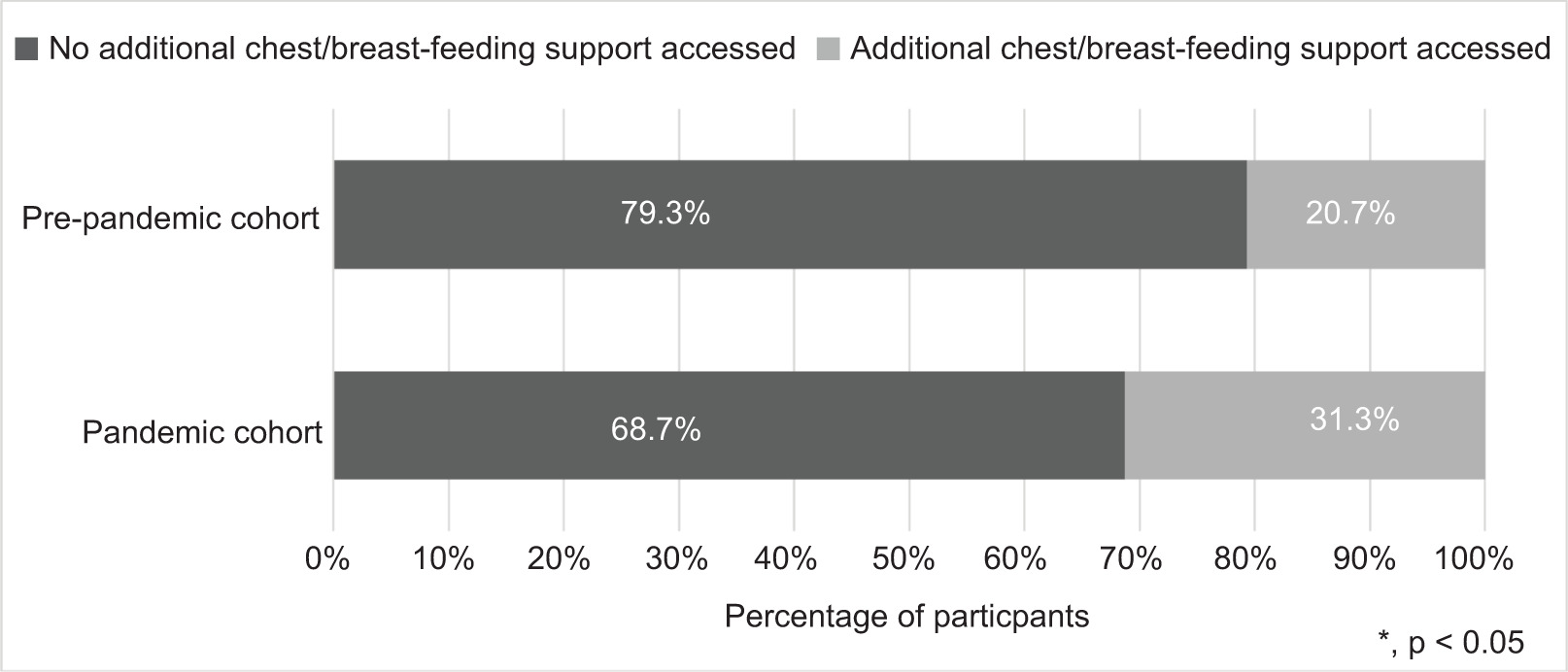
Additional Chest/Breastfeeding Support
In the pandemic cohort, there was a statistically significant 10.7% increase in clients who accessed additional chest/breastfeeding support from lactation consultants or pediatricians (Figure 2). In addition, we found there was a statistically significant increase in the number of clients with no prior chest/breastfeeding experience in the pandemic group compared with the pre-pandemic group; 56% and 39.3%, respectively (Table 1).
Figure 2. Comparison of additional chest/breastfeeding support accessed among the pre-pandemic and pandemic cohorts.
DISCUSSION
We did not find a statistically significant difference in exclusive chest/breastfeeding rates at 6 weeks postpartum in the pre-pandemic and pandemic cohorts in this study. The rate of exclusive chest/breastfeeding in the pre-pandemic group was 82.7%, while the exclusive chest/breastfeeding rate in the pandemic group was 74.7%. These numbers are slightly higher than the 2022 Ontario midwifery rate for exclusive chest/breastfeeding at 6 weeks (71%)22 and higher than provincial and national rates of exclusive breastfeeding at 2 months, 68.4% and 66.6%, respectively.23,24
One of the hallmarks of the Ontario midwifery postpartum care model is the multiple in-person postpartum visits in the setting of the client’s choice. Similar to the AOM’s Postpartum Visit Schedule Guideline18; a large 2022 Cochrane Review of 116 trials investigating effective chest/breastfeeding support found that four to eight visits for chest/breastfeeding support were associated with higher exclusive chest/breastfeeding at 4 to 6 weeks and 6 months.25 In this study, the midwives provided between four to eight in-person postpartum visits, averaging six postpartum visits before the pandemic (Table 2), which was in line with Ontario midwifery guidelines at that time.
The AOM’s “COVID-19: Reduced schedule of visits and use of PPE in midwifery contacts” guideline proposed two visits in the first week with additional visits by phone or videoconference.21 Interestingly, we found that the average number of postpartum visits in the pandemic cohort was unchanged, in spite of the recommendation to decrease the number of visits to reduce COVID-19 exposure and community transmission. Similarly, the type of visit did not change between the cohorts, and it was almost exclusively in-person in spite of the recommendation for virtual visits when appropriate. The 2022 Cochrane Review mentioned above found that the type of support: faceαtoαface, telephone, digital technologies, or a combination, did not significantly affect chest/breastfeeding rates.25 However, a study from the United Kingdom reported that 70.3% of participants attributed their decision for early chest/breastfeeding cessation during the pandemic to a lack of face-to-face chest/breastfeeding support.17 Parents in Canada who were able to access virtual chest/breastfeeding support during the COVID-19 pandemic unanimously viewed it as unhelpful.26
Midwives provide a full complement of postpartum care for both the birthing parent and infant. This unique model of care includes, but is not limited to, physical assessments such as blood pressure measurements and other vitals; perineal tear and c-section incision healing; initiation, establishment, and continuation of chest/breastfeeding support, including supplemental or formula feeding; newborn assessments, screens, medications, and prophylaxis; mental health support; and parent–infant bonding support. Many of these aspects of care would have been more difficult to provide using the alternative reduced visit schedule.
Other Ontario perinatal care providers have reported difficulties in providing standard clinical care virtually, such as the inability to perform physical assessments or hands-on emotional support.26 They asserted that virtual care could not substitute in-person clinical care.26
The midwives in this study provided frequent in-person postpartum visits to effectively assess and support clients’ and newborns’ well-being in spite of the recommended reduced visit schedule during the COVID-19 pandemic. Midwives are supported by the CMO and AOM to adjust the postpartum visit schedule using clinical judgment and appropriate health precautions.18,21 A recent study examining midwifery care in Ontario during the COVID-19 pandemic showed that midwives adapted protocols and guidelines to uphold the tenets of midwifery care during a crisis.27 Similarly, the midwives in this study remained committed to meeting the needs of clients during the COVID-19 pandemic and provided frequent in-person postpartum care visits while ensuring that health precautions were in place such as wearing full personal protective equipment, implementing health screening strategies for clients, and performing hand hygiene and appropriate cleaning of clinical equipment.
In spite of the number of postpartum visits provided remaining the same in both cohorts, we found a 10.6% statistically significant increase in additional non-midwifery chest/breastfeeding support accessed by clients in the pandemic group. Most of the clients who accessed additional feeding support in both cohorts were primiparous parents without chest/breastfeeding experience. The additional support was provided by lactation consultants and pediatricians. The pandemic cohort had a 16% statistically significant higher number of primiparous clients compared to the pre-pandemic group which could explain the increase in support accessed outside of midwifery care.
Lastly, we found that compared to the pre-pandemic cohort, the pandemic cohort had a higher rate of home births. There was a 9.3% statistically significant increase in SGMT midwife-attended home births between April and November 2020. This was likely because of clients’ desire to avoid COVID-19 exposure in clinical settings. Similarly, Ontario-wide data showed an increase in midwife-attended home births, peaking at 16.6% in May of 2020.28 Increases in out-of-hospital births may contribute to the initiation of and establishment of chest/breastfeeding because of reduction in interventions, increased skin-to-skin and decreased disruption of the parent–infant dyad.
CONCLUSION
The high exclusive chest/breastfeeding rates of midwifery clients in Ontario have been attributed to the midwifery postpartum care model which provides individualized care for the parent– infant dyad. The COVID-19 pandemic resulted in many restrictions that affected the provision of midwifery care. Midwives in Ontario were advised to decrease the number of postpartum visits as well as to replace in-person visits to virtual encounters when appropriate to reduce the exposure and transmission of the COVID-19 virus. Midwifery clients and midwives in this study demonstrated a high commitment to exclusive chest/breastfeeding before and during the pandemic. The pandemic cohort in this study was found to have similar exclusive chest/breastfeeding rates as the pre-pandemic group. When we looked at the postpartum visits provided by the midwives, we found that the midwives did not reduce the number of visits nor the number of in-person visits for clients. Midwives are supported by the CMO to use clinical judgement and expertise in postpartum care when devising individualized postpartum care plans for clients. The midwives used a multiple in-person postpartum visits model to meet clients’ needs, demonstrated by similar high exclusive chest/breastfeeding rates in the pre-pandemic and pandemic groups.
LIMITATIONS
This study’s main methodological limitations are that the data were collected from one midwifery practice group in Toronto and during the first 10 months of a multiyear pandemic with constantly changing health recommendations and restrictions. The results may not be generalizable to other midwives in Canada because of differing models of midwifery postpartum care across the country. Future research on the Ontario midwifery postpartum care model, how it has been transformed by midwives during and since the COVID-19 pandemic, and how midwives determine the need for postpartum care would provide more insight into the excellent exclusive chest/breastfeeding rates and other health outcomes of midwifery clients in Ontario.